An elective surgical treatment called deep brain stimulation (DBS) involves implanting electrodes in specific parts of the brain. Electrical impulses produced by these electrodes, sometimes known as leads, are used to regulate aberrant brain activity. The chemical imbalances in the brain that lead to various illnesses can also be corrected by electrical impulses. A programmable generator that is positioned beneath the skin in the upper chest regulates the stimulation of various brain regions.
Three distinct parts make up the DBS system:
- The electrode, often known as the lead, is a thin, insulated wire that is implanted into a particular part of the brain through a small incision in the skull.
- Connecting the electrode to the internal pulse generator is the extension wire, which is also insulated and runs underneath the skin of the head, neck, and shoulder (IPG).
- The third component of the system, the IPG, is typically implanted in the upper chest under the skin.
To treat patients with movement problems such as essential tremors, Parkinson’s disease, and dystonia, doctors often perform deep brain stimulation (DBS) surgery. Obsessive-compulsive disorder and epileptic symptoms can both be managed with it. When medication is no longer helpful in preserving a patient’s high quality of life, this treatment is used.
The Deep Brain Stimulation Procedure: Stereotactic Deep Brain Stimulation vs. Interventional Image-Guided DBS
In certain circumstances, the surgeon will implant the lead and the neurostimulator at the same time. In other circumstances, the two procedures may be carried out independently, with the neurostimulator being installed a few days or weeks after the lead is implanted.
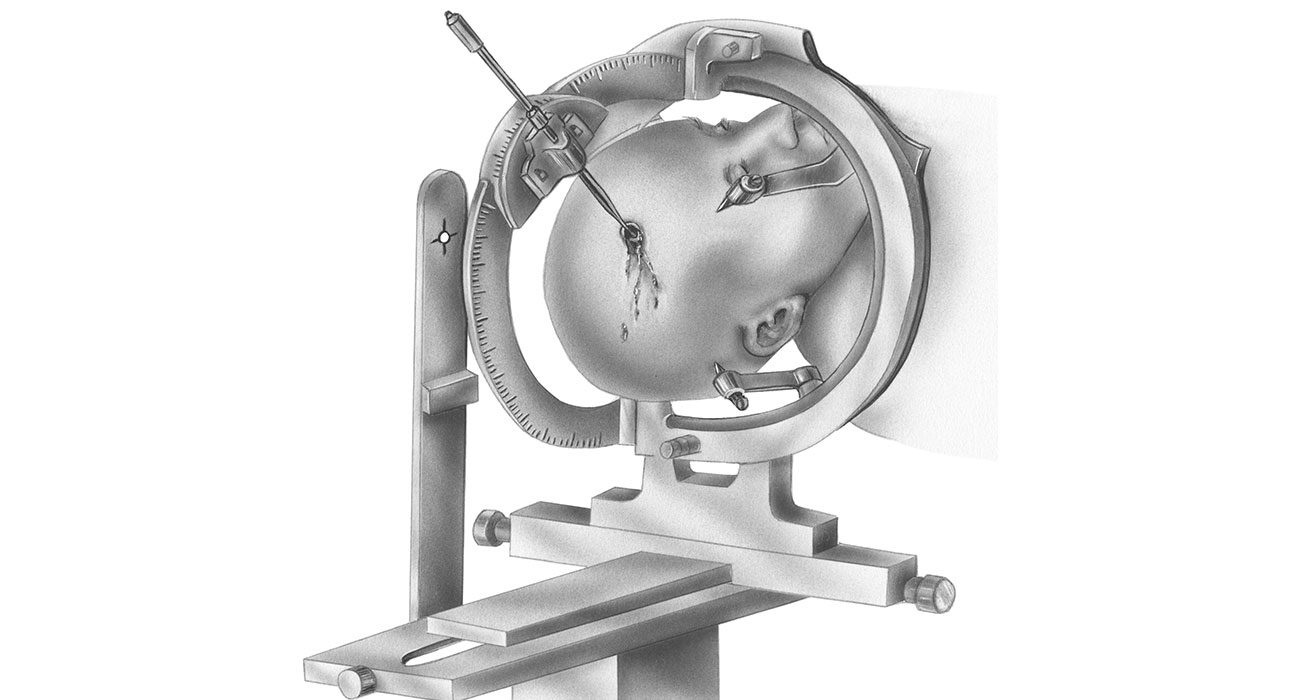
The patient must stop taking their medications before having stereotactic DBS surgery. A frame supports the head during the procedure and offers coordinates to assist the surgeons in directing the lead to the proper area of the brain. The patient is given a moderate sedative to help them unwind as well as a local anesthetic (numbing medication) to make them comfortable throughout each phase.
The patient is frequently sleeping and under general anesthesia during an image guided system of DBS surgery, such as with interventional MRI (iMRI) or CT scan, as the surgeon uses pictures of the brain to guide the lead to its target.
Stereotactic apparatus and iMRI-guided DBS procedures are both available in some cutting-edge hospitals. The best procedure in this situation will be discussed by the doctor and patient based on a variety of variables.
For patients who have severe symptoms, are extremely nervous or afraid, or whose leads enter specific regions of the brain, the doctor might advise an image guided intervention treatment.

DBS surgery typically goes through the following steps:
Lead Implantation
- The patient takes off any jewelry, clothing, and other anything that might get in the way of the treatment.
- The surgical team removes a little amount of hair from under the hairline before injecting local anesthetic (a numbing agent) into the scalp to prepare it for the head frame’s insertion.
- To maintain the head in the correct position during the surgery, the head frame (or “halo”) will be screwed onto the skull.
- The target region in the brain where the lead will go is then identified by the team using CT or MRI.
- The neurosurgeon drills a small hole in the skull to place the lead after administering further numbing medicine.
- To ensure precise insertion of the lead, the team documents the procedure as it passes through the brain tissue. While the recordings are being made, the subject might be requested to move their face, arm, or leg at specific intervals.
- The lead is connected to an external neurostimulator once it has been placed. The doctors use electrical stimulation delivered through the lead for a brief amount of time to see whether symptoms get better or whether adverse effects (such as muscular contractions or visual abnormalities) manifest.
- The lead is connected to the neurostimulator via an extension wire that is hooked to it and positioned beneath the scalp.
- With the use of sutures and a plastic cap, the skull’s entrance is sealed.
Microelectrode Recording
Using electrical current (5-100uA) at a very high frequency (300Hz), microelectrode recording (MER) can precisely pinpoint the surgical location for deep brain stimulator installation (DBS).
Because each person’s brain has a unique structure, the data from MER provides an accurate target for the placement of the DBS. The surgical team may see and hear the neuronal activity from various parts of the brain using the microelectrode, and they can use this information to recognize particular structures based on the distinctive patterns of neuronal activity. For MER to produce high-quality data, the patient must be awake (and not under general anesthesia).
Placement of the Neurostimulator
The patient is sleeping during this treatment since a general anesthetic is used. The neurostimulator is inserted by the surgical team beneath the outer layers of skin, frequently just below the collarbone but occasionally in the chest or belly. The neurostimulator is connected to the lead’s extension cable.
What Happens After Deep Brain Stimulation Surgery?
In the Hospital – A DBS patient will typically stay in the hospital for 24 hours, though this time frame may be extended depending on how quickly the patient heals and is prepared to go home. The doctor will check that the patient is prepared to go and give instructions for home care during the visit.
At home – It’s crucial to keep the incisions clean and dry at home. The patient will receive special instructions from the doctor on how to bathe while the surgery site heals. If stitches are necessary, they will be taken out during a subsequent office visit. If adhesive strips are used, they must be kept dry and usually peel off after a few days.
A magnet will be provided to the patient, who can use it to activate or deactivate the neurostimulator as directed by their physician.
References:

Leave feedback about this