
Before going into the depths of recent advances in DBS surgery, let us understand what is Deep brain stimulation (DBS) surgery. DBS is a neurosurgical procedure, that involves the implantation of electrodes in the target sites of the brain with a precision of 1 to 2 millimeters. These electrodes are in turn connected with the help of an extension wire to the pacemaker which ends up delivering current into the brain. The pacemaker is similar to the one which has been used for many years for cardiac surgeries. DBS surgery has been there around the world for more than 30 years now and has been widely used for treating diseases ranging from movement disorders including Parkinson’s disease; psychiatric disorders like depression and OCD; epilepsy, pain, and several other neurological conditions. The indications of DBS are ever-expanding as technological improvements occur and the understanding of the diseases that affect us becomes known.
For the last 20 years, there had been very little change and advancement in DBS technology. The basic DBS technology involved as described above, is the lead, extension, and pacemaker. The pacemaker was quite limited in its application to deliver the type of current. It had a fixed set of pulse width, frequency, and voltage that can be utilized and very little customizing was possible between different sites of the brain to be stimulated.
Recent Advances In The DBS Technology
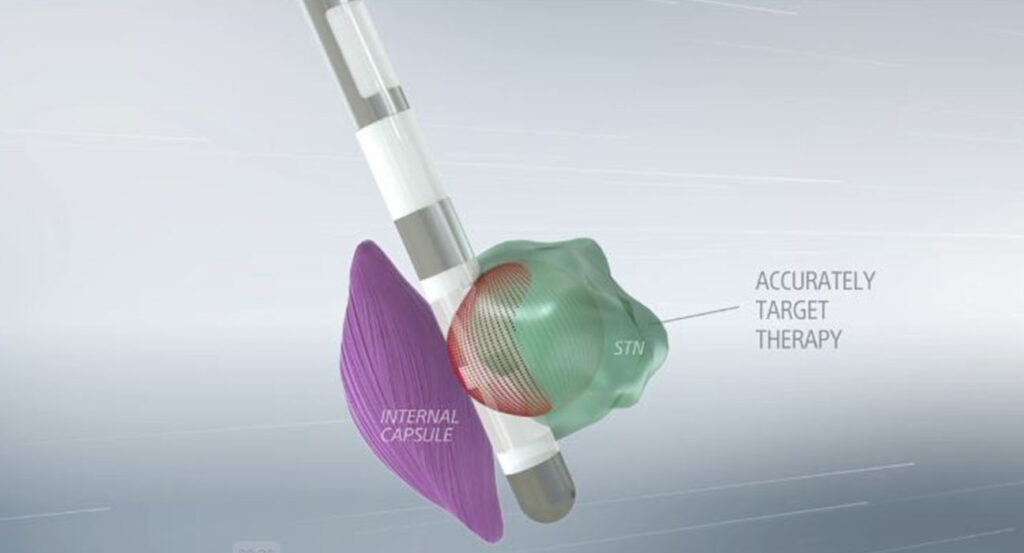
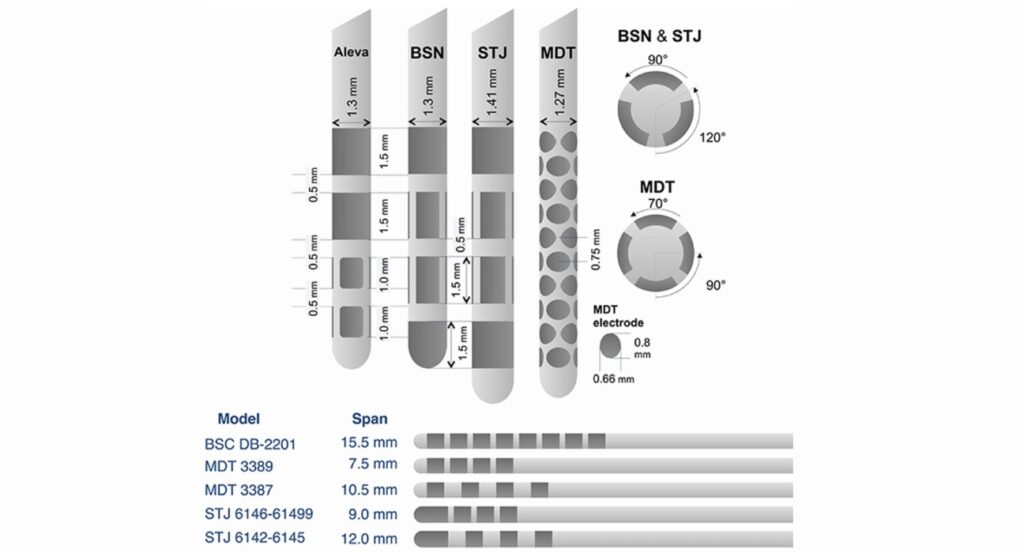
Directional Leads
Leads or the electrodes that go into the brain are the main component interface between the pacemaker and the target site. Over years the researchers found that by delivering the stimulation to the target sites some of the currents would spread to the unintended areas of the brain causing the side effect. And hence the researchers work to develop electrodes that could deliver the current in a particular direction. These are called directional electrodes. Essentially the conventional electrodes which were circumferential would deliver radial current all around symmetrically and as the current size would increase, so would the current and it spread to the desired and unwanted areas of the brain. The directional electrode has fractionated this segment of a circumferential ring into 3 segments interspersed with an inert material in between. Each segment of this fractionated ring would work as an independent contact point and hence can be used to deliver the current to the area that surrounds that contact point. With the help of this directional lead, we can improve the efficiency of the target stimulation and minimize the side effect by minimizing the current spread. The directional lead is not a substitute for substandard surgical skills but it only benefits marginally in improving the outcome.
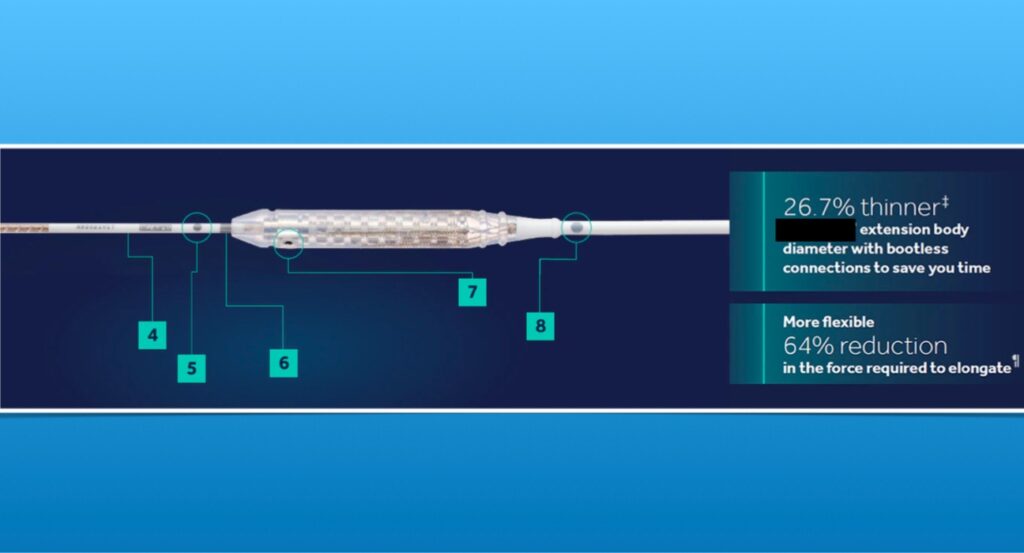
Extension Wires
These are the connecting wires that link the electrodes and the pacemaker. Over the years, clinicians found that one of the common sites of erosion was behind the ears where these extension wires were joined with the leads. Medical device companies have taken cognizance of this and have now developed low-profile extension wires which doesn’t put too much pressure on the subcutaneous tissue and hence minimize the risk of erosion. One of the other features of these extension wires was a pulling sensation or a tight band-like feel in the neck as a complaint by some patients. Once again the new extension wire have being able to mitigate this by allowing some level of elasticity built in and hence making it more comfortable for the patient.
Pacemakers
It is in this area that the maximum amount of innovation and research has been done. Over the last 10 years, the number of new designs of pacemakers that have come to the market has simply made it very confusing and difficult for clinicians to understand the capabilities of each device and also to maximize the application of this device. Having said that, it has become even more challenging to identify the right candidate that can benefit from the selection of the right kind of device. The pacemaker innovations have changed the way we stimulate the target sites in the brain and have given the immense power of flexibility to the clinician to tailor the treatment for each patient, and even in each patient for each side of the body, when they are stimulating different sides of the body for different diseases. Coupled with advances in lead technology, the modern-day pacemaker can be independently used as an individual pacemaker to deliver current through each contact point of the lead. Typically each lead has 8 contact points and 2 leads combined which would have 16 contact points, so it is not unfair to say that the modern-day pacemaker can house 16 independent pacemakers into one single pacemaker which can be utilized to deliver and function as an independent current source for each electrode contact point.
The other innovation has come in the form of recording brain signals and understanding the application of these brain signals in improving the therapy outcome. In Parkinson’s disease patients, we have found that local field potentials can be very useful in understanding the disease fluctuation. We now have a pacemaker that can record in real-time and continuously, these signals from the brain and provide the clinician an input as to how the stimulation therapy and the medication therapy are helping the patient.
A few years back it was not possible to perform an MRI on patients who have undergone BS; however, over the years, companies have designed new pacemakers which are now MRI-compatible. Most modern pacemakers are MRI compatible and patients can safely undergo MRI even after the implantation of the DBS system.
Takeaway
Above is the synopsis of the current advances that have occurred in the technology of DBS. There have been further advances in the types of rechargeable devices’ programming capabilities, understanding the volume of tissue activated and the current delivered to each target site of the brain, and many other areas of therapy which have led to a better and more sustained outcome in patients suffering from a neurological disorder.
About the Author: Prof. (Dr.) Paresh Doshi is a well-known stereotactic and functional Neurosurgeon at the Jaslok hospital and research center Mumbai. He is the pioneer in DBS surgery and he is at the forefront of technological advancement and research in the field of neuromodulation. Currently, he holds the position of President of the Neuromodulation Society.
References:
1. https://pubmed.ncbi.nlm.nih.gov/29503332/

Leave feedback about this