DBS (or deep brain stimulation) is a treatment intended for those exhibiting Parkinson’s disease symptoms, such as tremors, trouble walking, and stiffness. It is also efficacious in combatting the side effects of medicines prescribed for Parkinson’s disease. That said, DBS should not be considered as a cure for Parkinson’s and will not stop it from worsening. However, the procedure may be a viable option if you have had the disease for a minimum of five years, with no relief from medicine. DBS is aimed to significantly improving the quality of life.
What Is DBS?
The primary treatment for Parkinson’s is medications. However, you can opt for DBS if drug treatments gradually become less efficacious in easing out your symptoms.
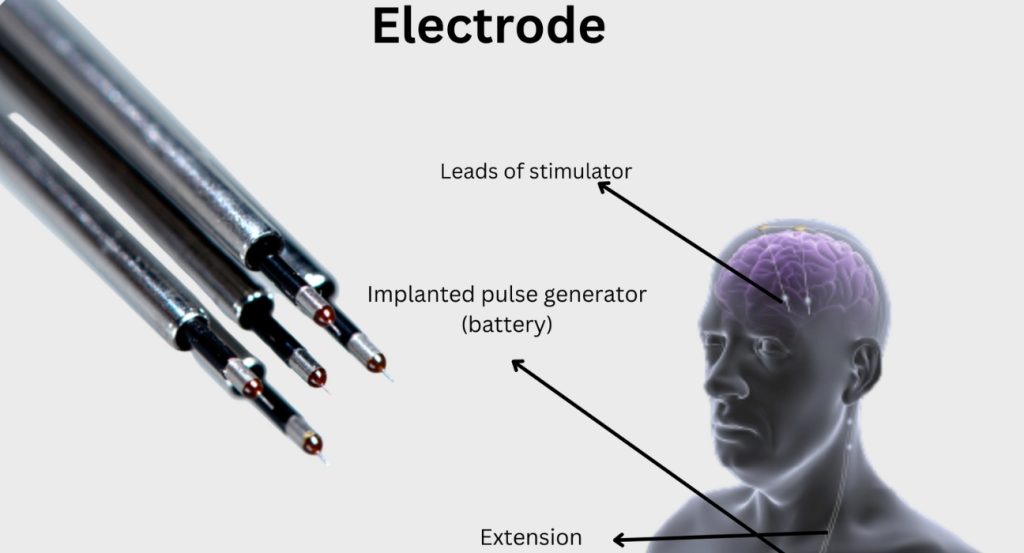
A pulse generator (which is a device that resembles a heart pacemaker) is placed beneath the skin, around the chest or stomach region. It is connected with precision to one or two fine wires that are inserted into specific regions of your brain.
After the pulse generator has been switched on, the implanted electrodes deliver high-frequency stimulation to the targeted region. This stimulation alters some of the brain’s electrical signals that cause the onset of Parkinson’s symptoms.
Purpose Of DBS
DBS could help if medications become less efficacious in easing out your symptoms.
DBS should not be viewed as a cure and does not successfully stop Parkinson’s from progressing. However, in many cases it has given individuals with the condition better control when it comes to their motor symptoms, including tremors, involuntary movements, and speed of movements.
Similar to all types of surgery, DBS involves certain risks. Make it a point to speak to your doctor to comprehend all complications that could arise due to the procedure. It has been shown that with experience the complications rate of surgery are reduced significantly. In a recently published article it was shown that the rate of complications significantly reduced after 300 surgeries.
Procedure Followed

DBS may be carried out slightly differently at each hospital or surgical centre. The team of doctors at your hospital will be able to offer you info about the specific procedure that you may need to undergo.
During the surgery, a frame will be fitted around your head to help in preventing movement during the procedure. Two, thin, insulated wires (each with electrodes also known as ‘contacts’) are inserted into the brain. In a rare scenario, when Parkinson’s symptoms primarily affect one side of your body, these leads are only inserted on one side your brain. The lead that is implanted on the brain’s left side will control symptoms affecting the body’s right side, whereas the lead that is implanted on the brain’s right side will control symptoms affecting the body’s left side.
There are several steps to help the surgeon guide the placement of electrodes in the brain. One of them is Microelectrode recording. These recording are like a signature of the cells where the electrode is to be implanted and hence improve the accuracy of the surgery.
Your surgeon will precisely implant the leads into a specific region of the brain that is effective for Parkinson’s: the position will vary from person to person. Post-surgery, you may be required to undergo a detailed scan (such as a CT scan) to ensure that the leads are placed spot on.
Based on the technique used, the procedure is either done and completed during one sitting or during two distinct operations. This may be the case so that the device can be implanted just a few days after the insertion of the leads.
Devices Used In DBS
There are numerous DBS devices available that help in transmitting the needed electrical current. These are known as neurostimulators or pulse generators. Different manufacturers produce different devices, and your team at the hospital will help in explaining which are readily available and the diverse advantages and disadvantages of each one.
There are some minute differences between each device, but the primary difference is that there are devices that are classified as rechargeable and non-rechargeable.
- Non-Rechargeable Neurostimulator
On an average, the battery life is between three and five years based on the needed settings. Certain batteries for non-rechargeable devices may eventually last longer than chargeable ones prior to a needed replacement.
- Rechargeable Neurostimulator
If the surgical team has used a rechargeable unit, you will be trained in using it. The neurostimulator will need regular recharging, and you will need to carry the recharging unit along with you if you are going to be out of your home for more than a few days. This battery will last approximately 15 years before it needs replacement.
To Sum It Up
Symptoms of Parkinson’s disease include tremors, stiffness, and trouble walking. DBS for Parkinson’s should be considered if medications have failed in controlling the symptoms. DBS also helps in taking care of side effects of certain medications for Parkinson’s. That said, it should be noted that DBS is not a cure for those with Parkinson’s.
References:


Leave feedback about this